What is Novomix?
novomix 30 is a modern fast-acting and intermediate-acting insulin (insulin analog) in a 30/70 ratio. Modern insulins are improved versions of human insulin. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . ............. ........................
How does it work?
The hypoglycemic effect of insulin aspartate is due to the fact that it facilitates the absorption of glucose by binding to insulin receptors in muscle and fat cells and at the same time that it inhibits hepatic glucose production.
NovoMix is biphasic insulin, containing 30% soluble insulin aspartate. It has a rapid onset of action, so it can be administered closer to a meal (0–10 minutes before or after the meal is started) than soluble human insulin. The crystalline phase (70%) consists of protamine-crystallized insulin aspartate, whose activity profile is similar to that of human NPH insulin.
When NovoMix is injected subcutaneously, the action begins 10-20 minutes after injection. The maximum effect is reached 1 to 4 hours after the injection. The maximum duration of the action is 24 hours.
What are the benefits of taking it?
NovoMix is used to reduce high blood sugar levels in adults, adolescents, and children 10 years of age and older with insulin-dependent diabetes mellitus (diabetes). Diabetes is a disease in which your body does not make enough insulin to control your blood sugar level.
NovoMix will begin to reduce your blood sugar level about 10-20 minutes after injection, peak at 1 to 4 hours after injection, and the effect lasts for up to 24 hours.
In patients with type 2 diabetes mellitus, NovoMix can be used in combination with diabetes tablets and/or with injectable antidiabetic medicinal products.
How do I use it?
When NovoMix is used in combination with diabetes tablets and/or injectable antidiabetics, your dose may need to be adjusted by your doctor.
Use in children and adolescents
NovoMix can be used in adolescents and children 10 years of age and older when it is preferred to use an insulin premix. Limited clinical data are available for children 6–9 years old. No data is available for NovoMix in children younger than 6 years.
Use in special patient groups
If you have malfunctioning of the kidneys or liver (kidney or liver failure), or if you are over 65 years of age, you should check your blood sugar more frequently and consult your doctor about changes in your insulin dose.
How and where to inject
NovoMix is injected under the skin (subcutaneous administration). You should never inject insulin directly into a vein (intravenous administration) or muscle (intramuscular administration). NovoMix is only indicated for injection under the skin. Ask your doctor if you need to inject insulin by another method.
At each injection, change the injection site within the particular area. The best areas for injection are the front of the waist (abdomen), the gluteal region, the front of the thigh, or the upper arm. Insulin will work more quickly if it is injected into the waist area. You should always regularly measure your blood sugar level.
How to use NovoMix
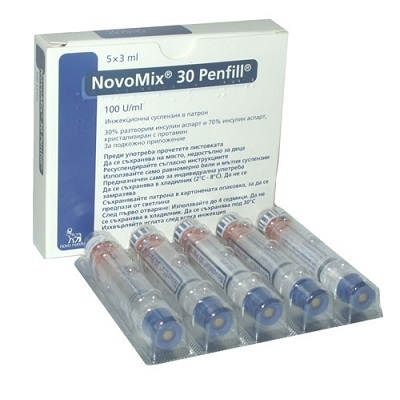
NovoMix is a color-coded, disposable pre-filled pen that contains a mixture of fast-acting and intermediate-acting insulin aspartate in a ratio of 30/70.
Always make sure you use the correct pen before injecting your insulin.
Its dosage
Dosage and when to take insulin
Always use insulin and adjust the dose exactly as your doctor has recommended. If in doubt, ask your doctor, pharmacist, or nurse again.
NovoMix is usually administered immediately before a meal. Take some food within 10 minutes after the injection to avoid a drop in blood sugar. If necessary, NovoMix can be administered shortly after a meal.
Do not change insulin unless your doctor tells you to. If your doctor changes you to another type or brand of insulin, you may need to adjust your dose.
When NovoMix is used in combination with diabetes tablets and/or injectable antidiabetics, your doctor may need to adjust your dosage.
Side effects & precautions
Like all medicines, this medicine can cause side effects, although not everybody gets them.
a) Summary of very frequent and serious adverse effects
Low blood sugar (hypoglycemia) is a very common side effect. It can affect more than 1 in 10 people.
Low blood sugar levels may appear if:
- Too much insulin is injected.
- You eat too little or skip a meal.
- You exercise more than usual.
- Drink alcohol.
Symptoms of low blood sugar: Cold sweat, cold, pale skin, headache, palpitations, nausea, excessive hunger, temporary changes in vision, drowsiness, tiredness, and unusual weakness, nervousness or tremor, feeling of anxiety, feeling confused, difficulty concentrating.
Severe hypoglycemia can cause you to pass out. If severe and prolonged hypoglycemia is not treated, it can cause brain injury (transient or permanent) and even death. You can regain consciousness faster with an injection of the hormone glucagon given by someone who knows how to do it. If you are given a glucagon, you should take glucose or sugary food as soon as you regain consciousness. If you do not respond to glucagon treatment, you will need to be seen in a hospital.
Uncommon side effects (They can affect up to 1 in 100 people).
Allergy symptoms: Local allergic reactions (pain, redness, hives, inflammation, bruising, swelling, and itching) may occur at the injection site. These usually disappear after a few weeks of treatment. If the symptoms do not disappear, you should consult your doctor.
Visual problems: When starting insulin treatment you may have problems with your vision, but this alteration is usually temporary.
Changes at the injection site (lipodystrophy): Fat tissue under the skin at the injection site can be reduced (lipoatrophy) or increased (lipohypertrophy). By changing the injection site each time insulin is administered, you reduce the risk of developing these skin changes. If you notice that your skin is depressed or thicker in the injection area, talk to your doctor or nurse. These reactions can become more severe or can affect the absorption of your insulin if you inject it there.
Inflammation of the joints: When you start insulin treatment, fluid retention can cause inflammation of the ankles and other joints. This effect usually disappears quickly. If not, check with your doctor.
Diabetic retinopathy (a diabetes-related eye disease that can lead to vision loss): If you have diabetic retinopathy and your blood sugar level improves very quickly, retinopathy may get worse. Consult your doctor.
Rare side effects (They can affect up to 1 in 1,000 people).
Painful neuropathy (pain from a nerve disorder): If your blood sugar level improves very quickly, you may experience nerve-related pain. This is called acute painful neuropathy and is usually transient in nature.








Reviews
There are no reviews yet.